By Staff
In a press release today WFBMC announced that Ocular Systems, Inc., Wake Forest Baptist Medical Center and the North Carolina Eye Bank have formed a new company based on a promising new technology aimed at engineering replacement corneas in the lab for transplantation. This is yet another step forward for our city which seems to be perpetually perched on the edge of a coming bio-tech boom.
“The global need for corneal tissue for transplantation far exceeds the supply,” said Dean Vavra, director of the North Carolina Eye Bank. “We are excited to be part of this innovative approach to sight restoration that has the potential to increase the availability of corneal tissue.” The new approach, not yet tested in patients, involves isolating cells from “banked” donor corneas to grow replacement corneal tissue in the lab. The advantage is that cells from a single donor could potentially benefit multiple patients with impaired vision.
The company, formed by OSI, the sponsor and initial funder of the project, Wake Forest Baptist Medical Center, whose Institute for Regenerative Medicine is conducting the research, and the North Carolina Eye Bank, is an example of the type of collaboration that is a strategic goal of the Piedmont Triad Research Park (PTRP). Also assisting with funding was the N.C. Biotechnology Center through a Collaborative Funding Grant.
The goal of the startup company, known as HCEC, LLC (Human Cultured Endothelial Cells), is to advance the technology to the next level, which includes conducting the additional studies needed to apply to the U.S. Food and Drug Administration to begin studies in human patients. This is expected to take several years.
“Today’s announcement is the culmination of more than four years of planning and research,” said OSI CEO Jerry Barker, who is the new company’s managing partner. “We believe this innovative initiative has the potential to change the face of corneal transplantation. The formation of HCEC, LLC will enable the team to expedite research and development efforts and move toward commercialization at a much faster pace.”
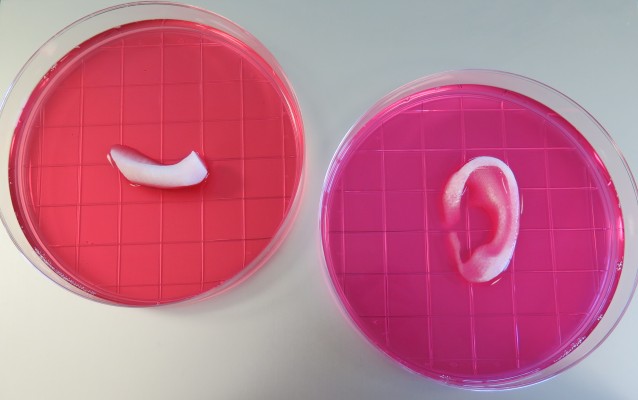
The cornea is the transparent dome at the front of the eye that helps with focus. The cells that line the inside of the cornea, known as corneal endothelial cells (CECs), pump fluid out of the cornea. If these cells become diseased or damaged, vision is blurred. Because CECs cannot repair themselves, the standard treatment is to replace the cornea or cells with tissue from a cadaveric donor.
The current surgical technique is to replace a patient’s damaged CECs with a very thin layer of tissue containing cells from a cadaveric donor cornea. The new cells pump fluid out of the cornea, restoring corneal clarity. With the advent of this procedure, there has been increased demand for donor tissue with healthy CECs. The goal of the new partnership is use regenerative medicine technology to meet this increased demand.
“The technique of bioengineering replacement tissues using cells and scaffolds can theoretically be applied to almost any tissue in the body,” said Anthony Atala, M.D., director of the Wake Forest Institute for Regenerative Medicine. “We are delighted to be OSI’s academic partner in this project.”
“It is exciting that a collaboration based in the Piedmont Triad research Park, right here in Winston-Salem, has the potential to create products that can bring benefits to patients throughout the world,” said Eric Tomlinson D.Sc., Ph.D., PTRP president and Chief Innovation Officer at Wake Forest Baptist. “This project is an example of the innovation that can be sparked in a research-park environment.”
Shay Soker, Ph.D., professor of regenerative medicine at Wake Forest Baptist, is the lead scientist for the project. Other team members are Tracy Criswell, Ph.D., instructor of regenerative medicine; Ocular Systems Inc. scientists Jin San Choi, Ph.D., and Belinda Wagner, Ph.D.; and Wake Forest Baptist Department of Ophthalmology physicians Craig Greven, M.D., chair, Matthew Giegengack, M.D., assistant professor, and Keith Walter, M.D., associate professor.
Editor’s Note: Wake Forest Baptist Medical Center and Keith Walter, M.D. receive royalties from OSI from sales of the EndoSerter® device, and Dr. Walter serves on OSI’s Medical Advisory Board and provides consulting for OSI.